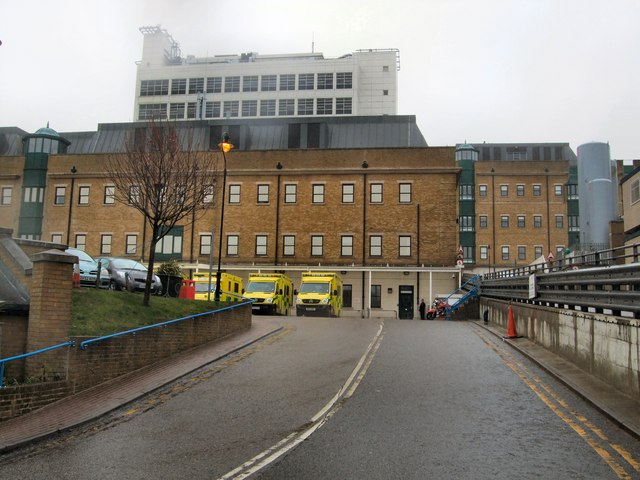
The new chief executive of Brighton’s main hospital trust said that up to £30 million will be spent upgrading Accident and Emergency (A&E) at the Royal Sussex County Hospital.
Marianne Griffiths, who takes over on Saturday (1 April), along with a team from Western Sussex Hospitals, said that some of the money would be used to tackle a maintenance backlog. Failing old lifts are an example of a recent problem area.
She said: “As part of the new management arrangements, healthcare regulator NHS Improvement will support the creation of a new emergency floor at the Royal Sussex County Hospital, designed to help reduce A&E waiting times and improve the quality and safety of urgent care services.
“Delivering a new A&E improvement plan is one of five key areas on which the new executive team will be focusing, along with moving the trust out of special measures on both quality and finance, progressing the hospital redevelopment project and building an organisational culture that can sustain improvement beyond the initial period of collaboration.”
Mrs Griffiths spoke about the extra cash as she and five fellow executives and Western chairman Mike Viggers prepare to take over the running of Brighton and Sussex University Hospitals (BSUH).
A management agreement to last a minimum of three years was signed last week.
Mrs Griffiths – named by HSJ (Health Service Journal) as Chief Executive of the Year four months ago – said: “The challenges faced by staff at BSUH have been well documented and there are no easy solutions to them.
“However, I have been hugely impressed by the welcome and openness extended to us by everyone. It’s quite humbling actually.

“I have seen enough examples of excellent care to feel that together we can bring about the improvements everyone wants to see.”
Mrs Griffiths, 56, started her career as a nurse before becoming a chartered accountant. She has a first class honours degree in psychology.
One of the members of her joint executive team, which will run the two trusts, is a former BSUH finance chief Karen Geoghegan. She spent 12 years at Brighton before leaving to become Western’s finance director in 2014.
The other members of the new top team are George Findlay, medical director, Pete Landstrom, strategy and performance director, Nicola Ranger, nursing director, and Denise Farmer, human resources and organisational development director.
Mrs Griffiths said that a number of senior colleagues at Western were ready to step up and take on more responsibility as the new arrangement started.
This would help bring in a period of stability, Mrs Griffiths said, adding: “The churn in the executive leadership here (BSUH) has been quite unique – six chief executives in five years.
“We’re coming in with an established whole team. The reason we’ve been asked to do that is that we’ve run a successful organisation in the west.”

She acknowledged that the two trusts weren’t the same. But the challenges that she had overcome merging St Richard’s, in Chichester, with Worthing and Southlands to form Western and dealing with a £21 million deficit meant that she had relevant experience.
“We paid it back,” she said. “And we’ll deliver a surplus in Western this year of £10 million.”
The end of year deficit at BSUH is likely to be between £60 million and £70 million.
Mrs Griffiths said that the budget would have to be tackled but added: “I won’t do any slash and burn stuff. We’ve managed to agree an ‘ask’ that is do-able.”
And hand in hand with a financial recovery at a sustainable pace, she pledged a “patient first” culture, empowering frontline staff.
Since BSUH has been in special measures, it has come in for a great deal of external scrutiny. Mrs Griffiths said that she had agreed a breathing space with regulators.
They would all come together for one monthly monitoring meeting to assess progress, freeing the leadership and staff to get on with the job.
BSUH chief accountable officer Evelyn Barker, who is effectively the current chief executive, will become the organisation’s managing director under the new arrangement.

She said: “Marianne and her team have been very clear that the improvements made by Western Sussex Hospitals over the last few years have been achieved by giving frontline staff the freedom to make the changes they know will make the biggest difference to patient care – and they are committed to creating a similar environment here.”
Western is one of only five acute hospital trusts in England to be rated outstanding – the highest grade – by the Care Quality Commission. The CQC is the official watchdog for hospitals and health care.
Mrs Griffiths added: “We’ve known from the outset that helping our neighbour is the right thing to do but we have spent a lot of time over the last four months making sure it is an achievable thing to do, not just in terms of helping BSUH improve but doing so while continuing to build on the progress we have made at Western Sussex too.
“To be certain we can do that, we will be strengthening the leadership team within the trust and prioritising the three things we think will have the greatest influence on the future of our services – monitoring and maintaining our CQC standards, expanding our ‘patient first’ improvement programme and supporting the development of the Coastal West Sussex Accountable Care Organisation (ACO).”
The ACO is a new organisation of local NHS bodies as part of the Sustainability and Transformation Plan (STP) for the area.
Although the management agreement is for a minimum of three years, it is likely to face an early test next month when a CQC inspection has already been scheduled. If nothing else, it will give the new team and the existing staff an updated checklist of the challenges that they all face in caring for and treating thousands of local patients.






Dear Sir,
I have been a patient at this hospital for the last week in the vascular ward, level 8, Kemp Tower. There has been no working central heating since my admission. Despite daily reports to hospital management this still has not been resolved and patients lives and wellbeing are being directly put at risk as a result.
I have been compiling a detailed temperature log during my stay here which will be submitted as evidence of the complete failure of your duty of care to your patients.
As I’d hope you would appreciate maintaining the temperature of the wards to an acceptable level is a primary responsibility you have to your patients. This is particularly critical in patients with vascular conditions making the difference between life and death, retaining limbs or losing them.
Given how relatively little expenditure it would take to provide adequate temporary heating in the event that the contracted service staff are unable to repair the systems I find it disgusting that no adequate provision has been made. Staff are wearing winter clothes inside the ward, while patients and are left in open surgery gowns to suffer and health deteriorate.
I would appreciate your comment in relation to this matter. Has heating the hospital fallen foul of cost saving measures? What next, the reintroduction of candles in preference to lights?